
My trip to Uganda as a Midwifery student
My trip to Uganda as a Midwifery student
This incredible place offered the most amazing worldwide experience as well as enhancing my love for midwifery... I wish to return to Uganda in the future, it’s the people I want to return to: the smiles and waves on our daily walk to work, the friendly staff at Kasangati Health Centre and the amazing midwives.
I chose to work three weeks in Kampala by myself alongside four other student midwives from the UK, I had no expectations or any preconceived ideas of what to expect and WOW… My placement was organised by a UK charity called Knowledge for Change, which is supporting Kasangati and other health facilities in Uganda to improve healthcare provision for mothers and patients through research and raising awareness.
My first day in Uganda
My first day was eye opening, I worked on the Labour suite alongside RM Dorti. Labour suite was made up of four beds and one cot, where a baby lay.
In the UK we have been taught to monitor women from the beginning of labour closely in a hospital or midwife-led home environment. Labour in the UK is private, planned far in advance and organised to create the safest environment we can for women. I quickly discovered how different labour can be in Uganda. Women at the beginning of their delivery journey, laboured outside of the health centre, and this wasn’t just at home, but outside of the centre itself and returned when they had the urge to push, they came in to the labour suite.

The reasons for this could have been cultural and socio-economical due to lack of space. Our first lady came in ready to push. I was so surprised to learn that the women were their own mobile pharmacies, bringing their own labour items to prepare them for delivering…
This included:
- A plastic sheet
- A bucket
- Four packs of sterile gloves
- A razor blade
- A large metre roll of cotton wool
- Four baby blankets with baby clothes.
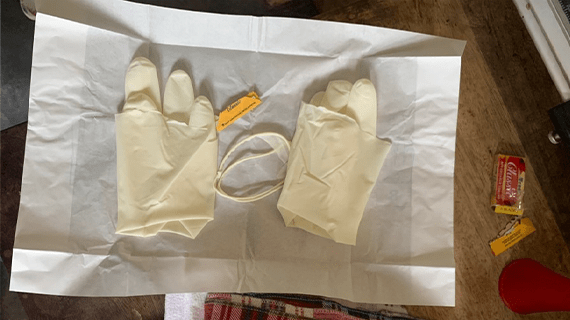
The plastic sheet was positioned over the bed, she passed urine in her bucket and got up on to the bed and started pushing. I said to Dorti ‘What should I prepare for the delivery?’ She took me over to a small table in the corner of the room. She opened one pack of sterile gloves and tore the wrist bands off each glove, placed them on the now not so sterile packet and opened the razor and said ‘OK we are ready’ I could not believe it… I started laughing, after a year of working in maternity trying to learn the ways of each mode of delivery having no idea what needle was for what or which equipment went where…… to ONE pack of gloves and a razor. I’ll never forget that moment. The picture you can see at the bottom shows our preparation.
The woman progressed quickly, which was at no surprise given the amount of time they spent outside of the hospital already in labour, vomiting in the same bucket she had used to go to the toilet. Her attendee, a choice of being more than often a female relative or friend, disposed of the contents and brought it back. I stood with the woman holding her hand and with each contraction we would say ‘Sindica’ (push). As the vertex became visible, we told her to breathe, put on our sterile gloves and mum delivered a beautiful baby boy. We passed him over, for skin-to-skin contact. A much smaller than UK dosage of oxytocin was given, and we waited.

I looked to Dorti in this time and said “is there something you’d like me to do?” She said ‘No, there is no bleeding so far, we have no reason to cut the cord and we need to do skin-to-skin for at least 30 minutes. The room was calm, the mother was calm and quiet and we enjoyed this amazing moment. We then cut the cord with the tiny blunt razor blade the woman had brought with her. We tied each end of the cord with the wrists of the sterile gloves we had ripped at preparation and continued with usual postnatal care.
It took me some time to come to terms with the ‘norm’ throughout this delivery. There had been no bedding used or pillow for the mother, only one plastic sheet. The cotton wool we used to clean the mother for suturing was not sterile, although this is requested to be sterile some women could not afford it and it was hard to get hold of. The curtains in the four-bed labour suite were not in use or broken so the privacy had been very minimal. This came as a shock to me with privacy being such a priority at home. It was then a new challenge to tackle other people’s presence (such as other midwives, doctors and several student nurses/midwives) in the room while concentrating on one birth. The clothes we dressed the baby in were too big and the blankets were thick fleece. I performed postnatal checks on the baby. Without equipment we had brought, there would have been no thermometer, no stethoscope to do those checks. If mothers wanted to have these checks more thoroughly, this was not an option. The hospitals were not equipped. A huge mixture of emotions.
Later that day I looked over to the baby laying swaddled in the cot in the labour suite – something didn’t look right. I had also seen no parents for this baby the whole morning, I knew something didn’t quite feel right here. A few moments later a Ugandan midwife walked in, she took the baby from the cot and put it on the bed beside her. She spoke a few words in Ugandan and I could tell by looking at his cold, grey skin this baby, now out of its swaddle had passed.


Dorti asked me to come out of the labour suit for my own emotional protection, she could have not been more concerning of my feelings, the level of emotional intelligence here was touching for their nurses. I felt ok but, out of respect for her consideration, did as she asked as they only had a cardboard box to transport the baby. I later asked her why this had happened, she explained to me, it had been a traumatic delivery and they could not get the mother to a better hospital in time. The baby had been in a poor state at delivery, and they were waiting to see what its outcomes would be.
We walked back to our accommodation, it had been a lot to take in all-in-one day, yet I felt so safe and supported. The midwives and staff within the charity constantly checked us for debriefs and did a big debrief each week on Friday afternoons.
The days slowly merged at Kasangati. I worked there for 3 weeks, we got experience in immunisations, cervical screening, antenatal and HIV clinics, Labour ward, postnatal ward and family planning. There were things that could have improved, things that had become the ‘norm’ over time, but even small acts made by us for example hand sanitation, creating more privacy for the women or providing comfort and encouragement through contractions were gradually picked up along the way by the staff and you could visually see it improve towards the end of our time there. The system cannot change overnight but the active efforts to improve women-centred care can. The most fascinating part of my trip was to see how they coped under such conditions and how very few staff coped with the amount of patients.

Throughout my experience in Uganda I was fortunate enough to not experience too many moments of emergency for mum and baby, however emergency’s did not feel so urgent. I had looked after a lady (one pictured) for several hours, she was not progressing and they decided to call an emergency C-section. I walked my lady over with help from her attendee (a friend) walked about 400m shoeless and contracting 3/10 over and dirt track up some stairs to the theatre. We then had to wait for the anaesthetist to arrive. I regularly went in to the theatre asking what was happening but as I did not know Ugandan there was very little I could do, I sat with my lady and comforted her as much as I could massaging through her contractions hoping I was helping. The C-section did not start till 2 hours after the call had been made. Ugandans don’t want medical intervention, birthing your child naturally they believed is a strong thing to do. You could see this when caring for women who needed intervention. I often went round to the new mothers and said ‘Kulika baby’ which meant congratulations and all the mothers would laugh – it clearly was not a common thing to say there! But they seemed to like it.

This incredible place offered the most amazing worldwide experience as well as enhancing my love for midwifery. In the two weekends I had off I managed to visit Jinja, the source of the Nile, white water raft, walk for 2hr’s in the rainforest. We managed two nights away on safari in the Pearl of Africa where we saw lions, warthogs, antelope, elephants, giraffes and many more amazing animals.
I wish to return to Uganda in the future, it’s the people I want to return to: the smiles and waves on our daily walk to work, the friendly staff at Kasangati health centre and the amazing midwives coping under conditions I didn’t know existed and safely delivering so many babies a day with nothing but their training and knowledge.
Most of all the staff we were working with had the knowledge for change, and there was not once I felt unsafe or unsupported and we could not have been better looked after. I was lucky enough to go with two beautiful second year midwives, Rebecca and Sally who had raised enough money to give back to Kasangati health centre. They used this for new curtains on the postnatal ward and labour suite (pictured), I’ll be forever grateful I was able to be a part of that.
Thank you, Dorothy, Claire, Annet, Allan & James and all the staff at K4C.


